Effective discomfort monitoring in the prehospital and emergency situation atmosphere is a craft as much as a proficiency. PUAEME008 Offer Pain Monitoring brings framework to that craft. The unit concentrates on evaluation, intervention, and continuous testimonial, and it sits at the intersection of scientific judgment, communication, pharmacology, and security. I have actually shown and examined numerous learners with this content over the years, from paramedic trainees to skilled registered nurses seeking to broaden their scope. The very same styles return every time: clarity in evaluation, precision in application, respect for danger, and ruthless reassessment.
This write-up unboxes what the PUAEME008 give discomfort monitoring unit expects in practice, how an offer pain management training course normally runs, and exactly how specialists in various roles can use it to develop their discomfort administration training. Whether you are exploring brief training courses in pain administration for acute treatment or aiming for a discomfort management accreditation training course that lines up with ambulance sector structures, you will find practical details here.
The clinical stakes
Untreated or undertreated pain is not just cruel, it has effects. Discomfort boosts sympathetic drive, elevates heart price and high blood pressure, and fuels anxiousness. In the injury person it can exacerbate blood loss. In older grownups it adds to delirium. In children it undermines trust fund and complicates future procedures. On the other hand, badly selected or extreme analgesia can depress ventilation, unknown developing pathology, or create hemodynamic instability. PUAEME008 shows that balance: deal with pain as the 5th essential sign while protecting airway, breathing, and circulation.
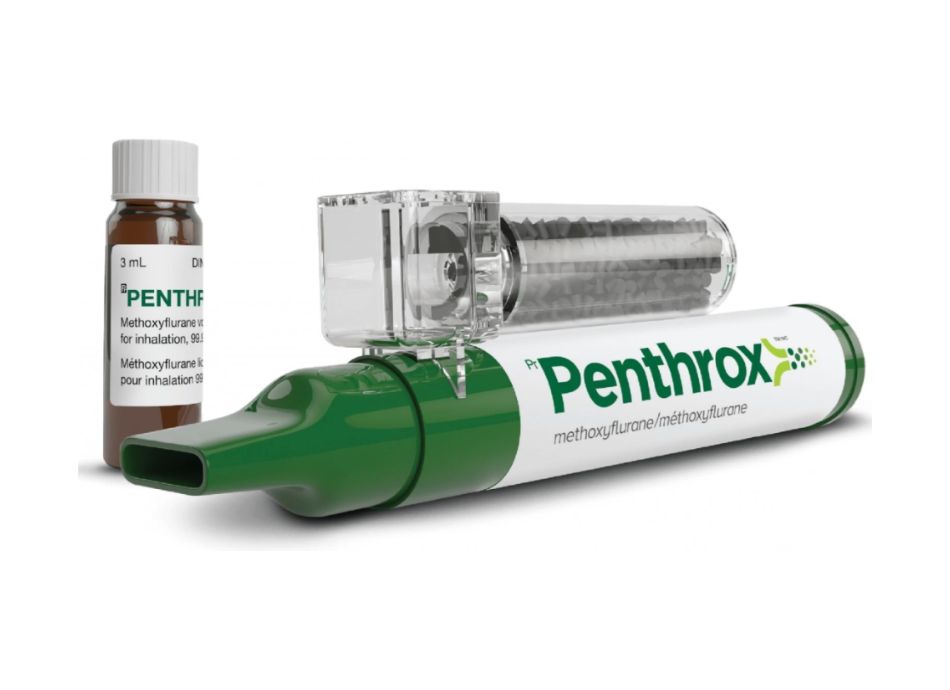
I remember a rural motor vehicle rollover where the first-on -responder was a volunteer with limited pharmacological options. They had actually training aligned with PUAEME008. With methodical assessment, they made use of non-pharmacological techniques and titrated inhaled methoxyflurane while waiting for an innovative staff. The individual reached the ED with regulated pain, undamaged respiratory tract reflexes, and stable vitals. That result reflects the unit's core approach: examine, interfere attentively, evaluation, and escalate when needed.
What PUAEME008 really covers
The unit title is blunt: Give Discomfort Monitoring. Under the hood, it collections right into 3 domains.
Assessment precedes. Learners need to take a discomfort history with precision, map quality and personality, and anchor it to vitals and context. The device anticipates fluency with discomfort scales like numerical rating scales, Wong-Baker for children, and aesthetic analog devices, and the capacity to adapt when an individual can not self-report, for example using FLACC for preverbal youngsters or behavioral discomfort ranges for the intubated. It likewise requires situational evaluation: mechanism of injury, red flags suggesting time-critical pathology, and ecological aspects that may influence both discomfort and the plan.
Intervention covers both non-pharmacological and pharmacological devices. Non-pharmacological techniques are never ever just extra padding in this system; they matter. Positioning, splinting, ice or warm where suitable, verbal peace of mind, and active interruption have quantifiable results. Pharmacology then layers on: breathed in analgesics like methoxyflurane, nitrous oxide/oxygen blends where readily available, oral representatives such as paracetamol and advil, and parenteral alternatives like fentanyl, morphine, or ketamine depending on the specialist's range and regional methods. The device does not turn every trainee right into a sophisticated life support paramedic. It educates secure, evidence-consistent choices within scope.
Review is not a token step. The device bakes in review periods and the assumption of outcome measurement. Did the discomfort rating drop within minutes of the intervention? Did respiratory system rate or end-tidal carbon dioxide change? Are sedation ratings drifting up? If you can not show improvement or you spot very early unfavorable impacts, you need to change the strategy quickly.
Who needs to consider this pain administration course
The target market for PUAEME008 is broad, which is part of its toughness. It is often packaged as an offer pain monitoring training course within emergency medical feedback programs and trade certifications that feed into ambulance assistance duties. It additionally appears in pain management training for nurses that work in immediate treatment, occasion medicine, or rural and remote centers. Lots of physio therapists finishing discomfort monitoring programs for physiotherapists wish to connect manual therapy and acute analgesia skills, specifically in sporting activities or job-related setups where initial action matters.
If you already hold a discomfort management certification or a broader pain management accreditation that focuses on chronic pain, PUAEME008 will really feel more tactical. The emphasis is on emergency discomfort monitoring, intense analysis under time pressure, and short half-life medicines that are titratable with a fast beginning. For clinicians that mostly see postoperative or chronic pain, this supplies a complementary ability set.
What a training course looks like in practice
A top quality pain monitoring training course that provides PUAEME008 usually runs as a combined program. Expect pre-reading on analgesic pharmacology and pain physiology, adhered to by an intensive day of case-based circumstances, skill stations, and simulated clients. Programs differ, however the exact same spinal column appears over and over: high-fidelity rehearsal of analysis, measured use medicines, and intentional emergency pain management experiment monitoring and communication.
Training carriers that take it seriously will analyze not just technical actions, but exactly how you speak to patients, translate pain ratings, and justify dosing decisions to a clinical lead over the radio. If you are selecting amongst discomfort management courses, ask the number of circumstances they run per student, what surveillance tools they use, and whether they cover pediatric and senior citizen adaptations. Excellent short courses suffering administration will include challenging cases: the intoxicated trauma client, the hypotensive abdominal pain, or the patient with a substantial opioid tolerance who needs rising dosing and a safety and security net.
Understanding pain past the score
Pain is subjective, personal, and culturally moderated. Two clients with the very same crack can report discomfort scores at opposite ends of the range. That does not make one of them incorrect. Your task is to secure the patient's summary of pain to function and to objective dangers. Can they take a full breath? Can they tolerate minimal activity for product packaging and move? Is the discomfort stopping you from doing essential procedures?
PUAEME008 motivates structured inquiry. Where is the discomfort, and does it emit? What makes it even worse or far better? What are the associated signs? In chest pain, inquire about diaphoresis, nausea or vomiting, lack of breath. In stomach discomfort, clear up location, beginning, and includes that distinguish medical from medical causes. In musculoskeletal injury, try to find defect and neurovascular concession. These details inform the analgesic strategy just as high as the number on the discomfort scale.
Non-pharmacological methods worth mastering
When people photo emergency pain administration, they assume syringes and inhalers. The quieter victories typically come from the basics. I have seen patients change from a pain rating of 8 to five in two mins with nothing more than mindful splinting and repositioning. An arm sustained in a sling reduces grip on damaged tissues. A broken shin in a well-applied vacuum cleaner splint ends up being bearable sufficient to enable mild transportation. Cold packs assistance in acute strains and contusions by decreasing swelling and numbing surface nerves. Warmth makes sense in muscular tissue convulsion, not in fresh trauma.
Communication belongs to the analgesic strategy, not a second thought. Discuss what will certainly occur, what sensations to anticipate, and what you need from the client. Teach paced breathing for the next 2 mins while you prepare medications. In pediatric situations, engage the caretaker and use interruption devices. Also as you deal with the discomfort, you are gauging the action min by minute.
Pharmacology within scope and context
The exact medicine embeded in a PUAEME008 supply discomfort monitoring training course depends on territory and company range. The typical string is a tipped, titratable approach.
Inhaled options are a staple since they have a fast beginning and disappear promptly. Methoxyflurane can provide purposeful alleviation with marginal tools. It needs interest to application limits, advancing exposure, and a dedication to fresh air flow to decrease job-related exposure. Nitrous oxide 50 percent in oxygen gives trusted analgesia with a benign account yet needs cylinder logistics and keeping an eye on for nausea or vomiting, dizziness, or diffusion hypoxia if misused.
Oral representatives are in some cases ignored in urgent treatment, yet they have value, particularly when the individual is stable and transport times are prolonged. Paracetamol and advil utilized with each other can produce additive impacts. They are not sufficient for significant trauma, but they lower the opioid worry and can reduce rebound discomfort later.
Parenteral opioid choices often center on fentanyl and morphine. Fentanyl, with its quick onset and brief period, can be titrated in little increments. It has less histamine release than morphine, which aids when high blood pressure is breakable. Morphine provides deep, longer relief and can be reliable when offered meticulously with titration and monitoring. Both require mindful attention to respiratory condition, sedation, and collective application. Have naloxone readily available, yet do not rely on it to make up for inadequate decision-making.
Ketamine remains a valuable option where extent allows. In sub-dissociative doses, it provides potent analgesia with minimal respiratory system depression. It can increase high blood pressure and heart rate somewhat, which is preferable in specific injury contexts, and it preserves respiratory tract reflexes. Emergence sensations at reduced doses are unusual, yet still call for preparation and calm coaching. Incorporating low-dose ketamine with low-dose opioid can produce collaborating alleviation while minimizing the damaging profile of either medication alone.
Antiemetics and adjuncts issue. If the patient is wincing and vomiting, your strategy is not working. Ondansetron or comparable representatives support the experience. Little information like having suction prepared for an individual that comes to be sleepy can be the difference in between smooth care and a near miss.
Monitoring and safety and security nets
Every medicine choice rests inside a security framework. Prior to you begin, you confirm the essentials: license air passage, efficient breathing, adequate blood circulation. During analgesia, you view respiratory rate, oxygen saturation, and where available, end-tidal carbon dioxide. You keep in mind blood pressure and degree of awareness. Sedation scales offer you a language to explain what you see, as opposed to obscure words like sleepy or sleepy.
Good method suggests examining impact at details time factors. With breathed in anesthetics, you need to see meaningful adjustment within a few breaths and a steady degree within minutes. With IV opioids, initially inspect at 2 to 3 mins and again at 5 to ten mins before duplicating doses. Titration maintains you inside a therapeutic home window and constructs trust fund with the patient. Record the standard rating, the intervention, the time, and the brand-new score. This is not paperwork for its very own sake. It is how you learn what jobs and spot very early caution signs.
Special populaces and edge cases
Pain does not present nicely, and PUAEME008 anticipates you to adapt.
Children call for dosage changes, careful language, and tools like the Wong-Baker faces range. Splinting and adult participation can decrease distress considerably. Some inhaled representatives might continue to be off-label for really little ones, so your course ought to make clear local policy.
Older grownups process medicines in a different way. Decreased renal function, polypharmacy, and frailty enhance the risks of sedatives and opioids. Start reduced, go slow, and focus on non-pharmacological methods and local stabilization. A hip fracture patient usually takes advantage of well-padded positioning and mild grip, after that tiny aliquots of opioid or low-dose ketamine, always with oxygen and monitoring.
Pregnancy changes whatever from breathing get to hemodynamics. Positioning to avoid aortocaval compression, cautious oxygenation, and appointment with clinical control take priority. Certain drugs might be contraindicated relying on pregnancy. The system's guidelines will certainly defer to neighborhood procedures and assessment pathways.

Intoxicated or head-injured people pose a tracking obstacle. You can not rely on actions alone to judge sedation. In such instances, keep dosages tiny, reconsider pupils and ventilation typically, and preserve a low limit for sophisticated respiratory tract support if consciousness drifts. Pain still demands therapy, but the margin for mistake narrows.
Opioid-tolerant patients will certainly not reply to basic doses. It is very easy to undertreat them out of anxiety, then watch them move uncontrollably on a spine board. Titrate assertively while maintaining oxygen and respiratory tract equipment prepared. Low-dose ketamine can be indispensable below. Document their standard opioid usage; it justifies your application and guides handover.
Communication and handover
Clear, succinct interaction multiplies the worth of excellent clinical work. When you turn over an emergency discomfort management person, provide a timeline. For instance, you might claim that the individual's left wrist defect was splinted at 14:20, methoxyflurane began at 14:22, pain score fell from 8 to five by 14:25, and 50 micrograms of fentanyl IV were titrated in between 14:28 and 14:35 with a current discomfort score of 3. Add vitals, sedation degree, and any kind of damaging events. This narrative allows the receiving medical professional make sensible next actions rather than starting from zero.
Most pain administration training courses will certainly drill this type of handover. It might feel repetitive in the class, however it repays when your individual rolls into a crowded ED where focus is scarce.
Risk monitoring and legal considerations
Analgesia is not exercised in a vacuum cleaner. You function within business policies, medicine consents, and a progressing evidence base. PUAEME008 instructs you to confirm your extent, adhere to regional clinical practice guidelines, and inquire when offered with complicated or contraindicated situations. Documents is not simply defense, it is continuity of treatment. If you believe a medication is indicated yet the scenario deviates from typical methods, rise to a clinical lead, document the examination, and relocate carefully.
Environmental threats matter too. Utilizing methoxyflurane in a poorly aerated room rises job-related exposure. Carrying out nitrous oxide without scavenging can leave the crew lightheaded. Climate, darkness, and surface can turn easy jobs into threats. An excellent supply discomfort monitoring pain management certification for nurses course will certainly tip outside the class and reveal you exactly how to provide analgesia in a confined washroom, on a football area, or close to a street with traffic inches away.
How to select a top quality provider
Not all discomfort administration programs are produced equal. Try to find trainers with frontline experience, not just educating qualifications. Ask whether the course includes pediatric and senior citizen instances, air passage tracking skills, and unfavorable event management. Simulation should worry decision-making, not simply technical steps. The most effective discomfort management training courses supply post-course assistance, such as quick-reference application overviews and access to refresher scenarios.
If you are a registered nurse seeking pain management training for nurses, choose a supplier who comprehends nursing scope and common job setups. For physio therapists, find discomfort monitoring training courses for physiotherapists that incorporate movement-based approaches and splinting with analgesia concepts. Those working toward a discomfort management certificate or pain administration qualification need to guarantee the material maps to identified structures and consists of qualified analysis, not just attendance.
The useful flow at scene
Below is a small field-tested flow you can adapt. Maintain it honest and versatile, not rote.

- Scene safety and security, key survey, and immediate life hazards controlled. While you handle airway and bleeding, ask a single discomfort inquiry to set the stage. Focused pain assessment: area, quality, intensity, practical limits, red flags. Select a suitable discomfort scale. Non-pharmacological steps: setting, splint, ice or heat, calm mentoring. Beginning these before meds. Pharmacological strategy within extent: pick the most basic reliable representative, titrate gradually, display closely with recorded time points. Review at defined intervals. If the discomfort rating does not drop or negative effects show up, readjust the strategy or intensify for innovative support.
Building durable competence
Competence does not originate from a certificate alone. It originates from reps, reflection, and comments. After a challenging situation, assess it. Did you pick the right representative? Was your initial dose as well timid or as well vibrant? Did you reassess at the correct times? Speak with colleagues and teachers. The unit PUAEME008 offer pain administration expects reflective method. When you experience an uncommon unfavorable result or a stubborn discomfort syndrome that withstands your first-line options, compose it up and share the lessons with your team.
Consider routine refresher courses. Abilities like preparing small fentanyl aliquots under tension, mentoring a frightened kid via inhaled analgesia, or stabilizing ketamine's advantages versus periodic dysphoria get corroded without practice. Brief programs in pain management make good sense as yearly or biennial updates, particularly if your work environment modifications protocols or adds brand-new agents.
From certification to capability
A discomfort monitoring certification or pain monitoring accreditation looks neat on paper. What matters is how your patients experience your care. They do not bear in mind the unit code. They keep in mind the paramedic that splinted their leg gently, explained the strategy, timed each dose with their breathing, and remained present up until the discomfort reduced. They remember the nurse that located a comfy position for a fractured neck of thigh and used tiny, regular dosages to make movement manageable. They bear in mind dignity restored.
If you are evaluating whether to register in a pain administration certificate program, ask yourself what you want from it. If it is a badge, you will get one. If it is capacity, seek an offer pain administration program that makes you rehearse real-life intricacy, tracks your decisions, and offers honest feedback. The best program constructs your judgment, not simply your medication list.
Final thoughts for the field
Pain administration is a moral commitment and a professional skill. PUAEME008 offers a practical structure that stands in the unpredictable world of prehospital and urgent treatment. Utilize it to sharpen your analysis, broaden your treatments, and tighten your review loopholes. Respect the pharmacology, keep your monitoring truthful, and treat each client's pain as genuine, also when it presents in different ways than you expect.
The finest clinicians treat the individual before them, not a procedure laminated on a clipboard. They understand the guidelines all right to follow them and, when required, to securely request for aid when the guidelines do not fairly fit. That is the conventional worth going for when you lay out to provide discomfort administration in the minutes that matter.